
The World Health Organization describes work-related stress as having the potential to negatively affect an individual’s psychological and physical health - and an organization’s effectiveness. It’s a significant challenge to workers’ and organizational health world-wide.
Here’s a story about how Rachael, an administrative assistant, had trouble resolving her physical discomfort even after medical management and ergonomics. You’ll discover steps organizations can take to deal with complex workers’ comp claims.
The Story
Rachael is an administrative assistant for a government agency. She has worked with the same supervisor for the last five years and is constantly under her scrutiny. Over time, Rachael begins to fail to complete added assignments on time and meet routine deadlines.
Although relatively fit and healthy, she feels neck, upper back, and arm pain, especially during work hours, that gradually worsens over time. When the pain gets quite severe, she decides to report her discomfort to her supervisor. Rachael’s supervisor recommends that she go to the local occupational medical clinic.
During her visit, the doctor performs an examination. Her work injury diagnosis is relatively benign, with no significant or objective medical findings to explain the severe pain she’s had for the last year. The doctor determines that Rachael has no apparent loss of function. However, when asked about her discomfort level, she rates it as an 8 to 9 on a 10-point scale (0= none and 10=excruciating). As a result, the doctor prescribes a medical management plan for her, consisting of physical therapy, intermittent leave, task restrictions, and an ergonomic evaluation.;
Rachael complies with the medical treatment plan and has an ergonomic evaluation. The recommendations to help eliminate her neck and arm pain include a sit-to-stand workstation with a monitor arm to elevate her monitors to the correct posture in addition to other work practice strategies.
After several months, Rachael returns to the doctor, but her pain rating is only slightly better at a 6. While that is an improvement, she wonders what it’s going to take to get her discomfort level down to 0. What else could she do besides medical management plan and the improved workstation ergonomics?
Psychosocial Risk Factors
In this story, conservative medical management and good ergonomics are not enough to get Rachael well. What’s causing the discomfort and the ongoing workers’ compensation claim? When medical management and ergonomics is not enough, employers should explore the psychosocial risk factors at work.
If your employees are unhappy, in discomfort, or dissatisfied with their life or job, it will affect their health and well-being at work. Job stress, demands, support, and control at work may be to blame if workers’ compensation claims continue unresolved. The psychosocial work environment variables of high, demand, low control, and low social support are consistently associated with workers’ experiencing high strain and low well-being.
According to Karasek’s model (1979) (Figure 1.), job demands are the psychological stressors:
- Involved in accomplishing the workload.
- Related to unexpected task assignments.
- Associated with job-related personal conflicts.
- Of job control and decision latitude in day to day work tasks.
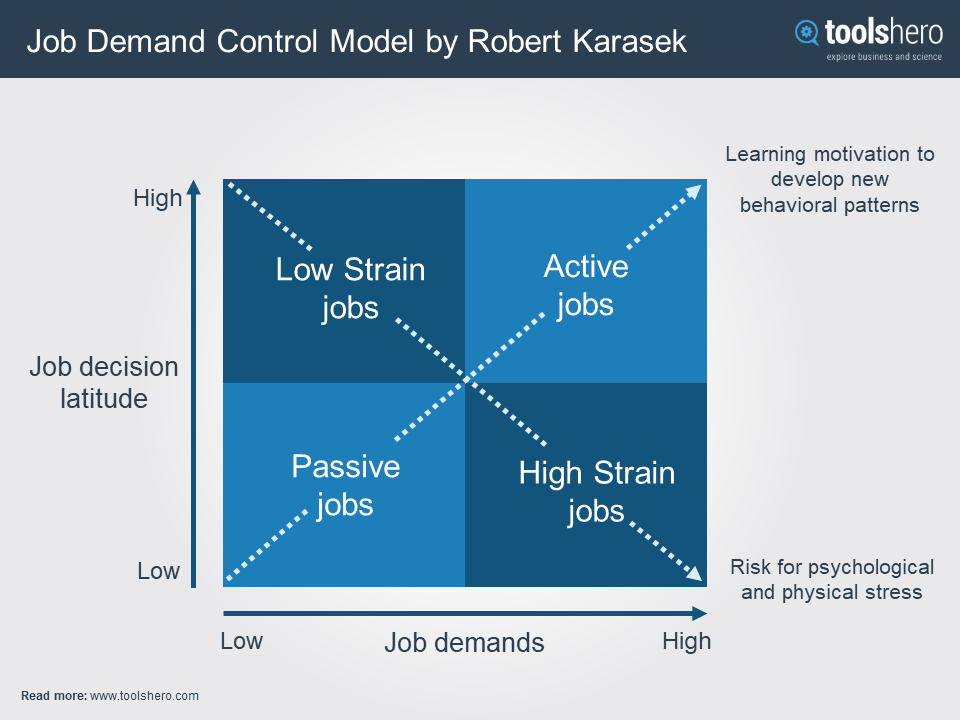
Figure 1. Karasak’s model of the of the Job Demand Control Model.
The combination of high job demand and low job control produce job strain, which can be associated with high discomfort levels often disproportionate to a diagnosed medical condition, such as an ongoing musculoskeletal disorder, like Rachael’s case. In such instances, the doctor is not likely to recognize it as contributing to the claim or document it in the medical record.
Psychosomatic pain is real, but often not acknowledged, especially in workers’ compensation claims. Employers should be willing to explore solutions focusing on the interactions between employee and supervisor as they may be hampering healing and wellness.
Steps Organizations Can Take
Based on the literature and my experiences dealing with similar cases, supervisors should:
- Engage and interact with injured workers sincerely regarding the performance of essential functions.
- Understand the importance of social support by providing employees with advice, assistance, and feedback on balancing work demands within their abilities and limitations.
- Provide helpful social interaction with co-workers, including them in committee or teamwork.
- Provide emotional support, empathy, and active listening to employee’s problems.
- Allow co-workers to assist with task completion when needed to reduce stress and work demands.
The impact of psychological job demands, job control, and social support are consistently found to be predictors of employee strain and well-being. Providing support, empathy and being more engaged in discussing work demands, workflow, and productivity with injured workers is critical if progress is not evident with typical ergonomic changes and medical management. Such actions will shift the balance of demands and control, allowing for reduced stress, discomfort and ultimately, return to normalcy, work/life balance and well-being.
So, what’s next for Rachael? More time off or restructuring her work demands giving her more control over her essential functions? Which option is likely to reduce her discomfort level and help resolve her workers’ compensation claim? Asking Rachael what will help is the best option for employers.
For support in dealing with complex workers’ compensation claims with psychosocial overtones, visit our Worker’s Compensation Services page.
The complexities of managing a workers’ compensation case have turned into the ultimate challenge for all those involved in disability management. The Ergonomic Worksite Analysis (EWA) demonstrates itself as a critical link in managing and helping to resolve many workers’ compensation cases with both physical and psychosocial risk factors. Click the link below to request a copy of this helpful white paper, Ergonomic Worksite Analysis: Critical Link in Return to Work/Stay at Work.

Comments (2)